- Home
- Women's Infections
- Bladder Infection
Bladder Infection, How You Got It, How to Treat It
Updated 6/24/2022
Medically Reviewed by Dr. Atmika Paudel, PhD - Written by by Dr. Shalaka Samant, PhD and Dan Jackowiak Nc, HHP
Dr. Atmika Paudel, PhD says... The facts and interpretation made in the article about recurrent UTI and its treatment are medically correct.
Bladder infections and UTI's are a very important factor to consider in treating chronic vaginal yeast infections since they are the second-most common reason women are prescribed antibiotics.
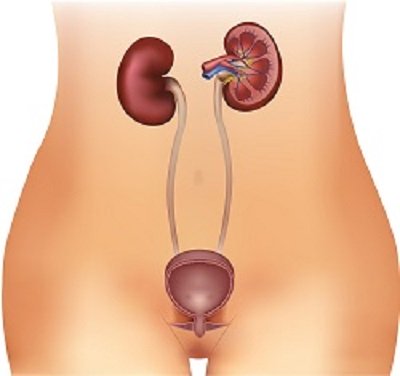
The typical symptoms can include a burning pain when urinating, increased urinary frequency, night-time urination, a turbid, foul smelling or dark urine, and lower abdominal pain.
90% of bladder infections and UTI's are caused by Escherichia coli bacteria. The remaining 10% of infections are caused by other species of pathogenic bacteria.
Symptoms must be correlated with a urine sample for the correct diagnosis. A microscope will reveal high levels of white blood cells and bacteria present in the urine.
How do You Get a Bladder Infection?
The microbiome of urine is different from that of the vagina and downstream body parts. As urine flows, it also gains bacteria from the vaginal microbiome. The body has many defenses to prevent growth of bad bacteria in the urinary tract.
The urine flow washes away bacteria, the pH of the urine prevents the growth of many bacteria, white blood cells control bacteria, and the lining of the bladder has anti-microbial properties.
Also present in the vagina and the intestines, are good bacteria. If this supply of healthy bacteria is altered or reduced, then Escherichia coli can enter the urinary tract through the vagina and multiply. Healthy bacteria in the vagina kill the bad bacteria by the releasing hydrogen peroxides and will not allow them to enter the urethra. These healthy bacteria also crowd out yeast and the bacteria that cause bacterial vaginosis.
High levels of Escherichia coli in the intestines, just like yeast, can transfer from the anus to the vagina quite easily. Reduce the good bacteria levels in the vagina and a urinary tract infection can be a result.
Women that suffer from bacterial vaginosis, which is caused by the Gardnerella vaginalis bacteria, have a greater risk of developing urinary tract and bladder infections. This trusted medical study was done at the Washington School of Medicine and published on Science Daily, confirmed that when Gardnerella vaginalis gets into the urinary tract, it triggers dormant E. coli to multiply leading to another uti.
Dr. Shalaka Samant, PhD says...
This article accurately describes the causes and natural means of treatment for bladder infections and Urinary tract infections (UTIs).
UTIs are a common clinical problem (1) across the lifespan of women. Recurrence of these UTIs (rUTIs) is another important consideration. The most common UTIs affect the bladder and the urethra. The E. coli infection is the most common type of infectious organism for the urinary tract. Although up to 90 percent of UTIs are caused by E. coli, the remaining 10 percent are caused by bacteria known as Chlamydia, Mvcoplasma, Neisseria gonorrhoeae, and others.
UTIs are the most common indication for antimicrobial use in hospitals (2). Antibiotics are great for knocking out the urinary tract infection causing microbe, but they also knock out the good microbes which can lead to overgrowth of yeasts, molds and ‘bad’ bacteria. UTIs can be caused by poor hygiene, impaired immune function, the overuse of antibiotics, the use of spermicides, and sexual intercourse.
The majority of rUTIs are believed to be re-infection from extra-urinary sources such as the rectum or vagina (3). UTIs most often occur when bacteria that live inside the bowel make their way into the urinary tract. The vagina is a key anatomical site in the pathogenesis of UTIs in women, serving as a potential reservoir for infecting bacteria and a site at which interventions may decrease the risk of UTI. The initial step in the pathogenesis of UTI is the colonization of the vaginal opening and area around the urethra (4) with the infecting pathogens, followed by their upward movement via the urethra to the bladder and sometimes the kidneys to cause infection.
Another cause of rUTIs, recently described, is the vaginal bacterium Gardnerella vaginalis which triggers E. coli (5) already hiding in the bladder to cause another UTI. Thus, understanding factors that affect the microbiota of the vagina is key to understanding the pathogenesis of UTIs and to designing interventions to prevent UTIs.
1. The Vaginal Microbiotia and Urinary Tract Infection. Microbiol Spectr. 2016 Dec; 4(6): 10.1128/microbiolspec.UTI-0025-2016.doi: 10.1128/microbiolspec.UTI-0025-2016
2.
Urinary Tract Infection and Asymptomatic Bacteriuria Guidance. Andrea
Green Hines MD, Mark E Rupp MD, and Trevor C Van Schooneveld MD.
Nebraska Medical Center, July 2014
3.
Management of Recurrent Urinary Tract Infections in Healthy Adult
Women. Duane R Hickling, MD and Victor W Nitti, MD. Department of
Urology, New York University Langone Medical Center,, New York, NY. 2013; 15(2): 41–48.
4. The Vaginal Microbiota and Urinary Tract Infection. Microbiol Spectr. 2016
Dec; 4(6): 10.1128/microbiolspec.UTI-0025-2016. doi:
10.1128/microbiolspec.UTI-0025-2016. Division of Allergy and Infectious
Diseases, Department of Medicine, University of Washington, Seattle, WA
98195
5. Transient microbiota
exposures activate dormant Escherichia coli infection in the bladder and
drive severe outcomes of recurrent disease. March 30, 2017
Natural Bladder Infection and UTI Treatment
The natural approach to treat bladder infections and UTIs can help prevent a vaginal yeast infection that can be caused by the antibiotics that are prescribed for this infection. The protective shield of beneficial bacteria that line and protect the urethra are stripped away when taking antibiotics and are usually replaced by less effective organisms.
Carol A. Kauffman et al, published a study in May of 2011 that said bladder and urinary tract infections caused by yeast are rare but do happen. If detected, follow up tests should be performed to determine species and if it is also in the bladder and possibly kidneys. As the above study points out, if it is in the kidneys, it needs to be treated or it can be fatal.
If you suffer from recurrent bladder infections or UTIs caused by bacteria, you should follow the suggestions below.
Increase your urine flow by drinking more liquids, ideally distilled or pure water. Herbal teas are ok and fresh juices diluted half and half with distilled water are ok unless you suffer from yeast infection also. If this applies to you, watch the sugar content. Avoid soft drinks, concentrated fruit juices, sweetened coffee, and alcoholic beverages. Drinking 16 ounces a day of natural, unsweetened cranberry juice has been shown to produce beneficial effects in 73% of men and women. Drinking more than that was found in tests to have very little effect.
D-Mannose is a simple sugar and close cousin of glucose and can cure more than 90 percent of all UTIs caused by E. coli within 1 to 2 days. Even more remarkably, D-mannose accomplishes this feat without killing a single bacterium!
Because it gets rid of UTI-causing bacteria without committing "bacteria-cide against good bacteria," people who use it suffer none of the unwanted side effects of antibiotics: no GI problems, no yeast infections, no resistant bacteria, and no mass slaughter of your good bacteria which can take a year to correct. In fact, D-mannose has no adverse side effects of any kind.
Itzhak Ofek and Edwin H. Beachey with the American Society of Microbiology found D-mannose inhibited or reversed E. coli epithelial cell adherence and yeast cell aggregation. Which could inhibit yeast from giving you a urinary tract or bladder infection.
As a bonus, D-mannose actually tastes good. Where a "spoonful of sugar" helped the medicine go down in Mary Poppins’s day, with D-mannose, a spoonful of sugar is the medicine. But it is not a sugar that yeast feeds on, it is a glyconutrient, so don't worry if you do have a yeast infection also, it won't feed it.
Because it is so effective and so benign, women (even pregnant women) who are susceptible to recurrent UTI’s can safely take D-mannose as a preventive measure to head off future attacks. D-mannose is also ideally suited for children with bladder infection or UTIs. Because it tastes so good, it is a sugar, after all, children actually enjoy taking it.
Although D-mannose is virtually unknown to practitioners of conventional medicine, many research reports have demonstrated its mode of action and effectiveness against E. coli, the microorganism that causes most UTIs. Moreover, nearly 15 years of clinical experience have shown that it is just about as effective at curing UTIs as antibiotic drugs.
At first glance, D-mannose may sound too good to be true: a "medicine" that’s highly effective, perfectly safe, pleasant to use, inexpensive, and available without a doctor’s prescription. Yet, it is true! Unlike virtually any conventional medication, and many natural or "alternative" treatments as well, D-Mannose has no known drawbacks and usually works within a couple days or less.
Doses for D-Mannose should be at least 3000 mgs per day.
Dr. Shalaka Samant, PhD says...
The holistic approach to treating UTIs includes the use of cranberry juice, increase of water consumption, reduced sugar intake, and probiotic supplementation. D-Mannose is by far the most effective supplement (6) for both treatment and prevention of UTIs. Similar to glucose in structure, D-mannose is a naturally occurring sugar that is found in a number of fruits, including apples, blueberries, and cranberries (7). This sugar is the reason that cranberry juice has been commonly recommended as a UTI treatment, though it is far easier to get the recommended dosage from a supplement.
D-mannose is effective because it attaches to E. coli bacteria, causing them to stick to each other (8) and preventing them from sticking to the walls of the urinary tract. The bacteria can then easily be eliminated from the body during urination. Some studies suggest D-mannose may play a useful role as a "prebiotic." Prebiotics are substances that may help your body by stimulating the growth of "good" bacteria in your digestive system.
D-mannose, even in large quantities, does not cause any adverse side effects (9), and cannot be metabolized the way other sugars can, making this supplement is safe for diabetics and others who are avoiding sugar for any reason. Patients who frequently feel like they are going to get a bladder infection after intercourse will do very well to try a teaspoon of D-mannose prior to intercourse.
6.
Oral D-mannose in recurrent urinary tract infections in women: a pilot
study. Journal of Clinical Urology. D Porru, A Parmigiani, C Tinelli,
... January 10, 2014 Research Article
7.
WebMD Medical Reference Reviewed by Melinda Ratini, DO, MS on February
05, 2020
https://www.webmd.com/vitamins-and-supplements/d-mannose-uses-and-risks
8. Effect of D-mannose and D-glucose on Escherichia coli bacteriuria in rats. Urol Res. 1983;11(2):97-102.
9. D-mannose: a promising support for acute urinary tract infections in women. A pilot study. Eur Rev Med Pharmacol Sci. 2016 Jul;20(13):2920-5.
Floraphage is a prebiotic supplement that feeds on harmful strains of E. coli that cause urinary tract infections. In doing so, it forces the E. coli to release its contents and these contents feed your good bacteria. As the E. coli is killed, it is swept from the intestinal wall which allows your good bacteria to take its place. Studies show it can increase good bacteria levels by 2400%.
Another good supplement for urinary tract infections is Uva Ursi here.
It works on a much broader range of bad bacteria than D-Mannose.
However, it could kill some of your good bacteria so I would make sure I took a probiotic while taking it. For additional information including studies, dosage directions and side effects of Uva Ursi, please see this webpage.
Taking a probiotic will also help build your good bacteria levels so you can prevent these infections in the future.
Dr. Shalaka Samant, PhD says...
Several studies have shown that changes in the characteristics of the vaginal microbiota resulting in the loss of normally protective probiotic bacteria (10) increase the risk of UTIs. Probiotic therapy to treat UTIs is an emerging concept, as it not only maintains low pH of the genital area, produces hydrogen peroxide and hinders the growth of E. coli but also activate the body’s innate immune responses (11) to target the pathogen.
10.
Reid, G., Bruce, A.W. Probiotics to prevent urinary tract infections:
the rationale and evidence. World J Urol 24, 28–32 (2006).
11.
Amdekar, S., Singh, V. & Singh, D.D. Probiotic Therapy:
Immunomodulating Approach Toward Urinary Tract Infection. Curr Microbiol
63, 484 (2011). https://doi.org/10.1007/s00284-011-0006-2
Make sure you have your urine monitored by your physician after 7 to 10 days.
By avoiding the antibiotics associated with most bladder infection treatments you will be able to avoid a vaginal yeast infection, which can be the result of taking these drugs.
Medically Reviewed by Dr. Atmika Paudel, PhD
Due to the anatomical structure, women are more prone to recurrent UTIs than men. Although not a part of the urinary tract, vagina plays a vital part responsible for getting UTIs. Associate other factors that increase the chances of getting UTIs are diabetes mellitus, pregnancy or other physiological and neurological disorders. The key to prevent and treat UTIs are keeping personal hygiene and following the approaches that help the body to maintain its normal flora so that bad bacteria and yeasts do not outgrow to cause UTIs. Therefore, diet and probiotic supplements, minimal use of antibiotics can help keep the balance of our urinary tract microbiome thus providing relief from the recurrent infections of the urinary tract.
D-mannose has been used as a safe alternative for UTIs as has been well mentioned in the above article. A recent paper published by Scribano et al. has experimentally verified the facts about D-mannose. They mention that D-mannose is safe to use, it can be well tolerated by the bladder cells and it provides least metabolic advantages for the bad bacteria as opposed to D-glucose, D-fructose or D-arabinose, other sugar sources (1). A randomized controlled trial in humans have shown also shown that D-mannose was better tolerated than antibiotic nitrofurantoin (2). Another review paper published recently in Nature Reviews Urology reviews about development of other synthetic mannosides. They require future clinical trials in humans but the data that have been obtained so far are promising. These synthetic mannosides have shown to have better in vitro and in vivo activity in animal models than D-mannose (3).
1. Scribano, D., Sarshar, M., Prezioso, C., Lucarelli, M., Angeloni, A., Zagaglia, C., Palamara, A. T., & Ambrosi, C. (2020). D-Mannose Treatment neither Affects Uropathogenic Escherichia coli Properties nor Induces Stable FimH Modifications. Molecules, 25(2), 316.
2. Kranjčec B, Papeš D, Altarac S. (2014). D-mannose powder for prophylaxis of recurrent urinary tract infections in women: a randomized clinical trial. World J Urol., 32(1):79-84. doi: 10.1007/s00345-013-1091-6.
3. Sihra, N., Goodman, A., Zakri, R. et al. (2018). Nonantibiotic prevention and management of recurrent urinary tract infection. Nat Rev Urol 15, 750–776.
Have Any Questions About Bladder Infections?
Do you have any questions about bladder infections or yeast infections in general? Ask your question here or contact us using the contact page of this website. It is also always a good idea to talk to your doctor as well.
Questions From Other Visitors
Click below to see questions from other visitors to this page...
Is D-Mannose safe to take during pregnancy? 




My wife recently developed a UTI during the first trimester. Her doctor prescribed the antibiotic fosfomycin as she is allergic to penicillin. We would …
What is your recommended dose of D-Mannose daily? 




What is your daily recommended dose of D-Mannose for bladder infections?
Back to Women's Yeast Infection
Home Privacy Policy Copyright Policy Disclosure Policy Doctors Store
Copyright © 2003 - 2025. All Rights Reserved under USC Title 17. Do not copy
content from the pages of this website without our expressed written consent.
To do so is Plagiarism, Not Fair Use, is Illegal, and a violation of the
The Digital Millennium Copyright Act of 1998.