- Home
- Systemic Infections
- Crohns Disease
Crohns Disease, Irritable Bowel Syndrome & Yeast Infections
Updated 1/24/2021Medically reviewed by Dr. Vibhuti Rana, PhD - Written by Dan Jackowiak Nc, HHP and Dr. Atmika Paudel, PhD
Dr. Vibhuti Rana, PhD says... The information below regarding the role of yeast infections in Crohn’s disease and Inflammatory Bowel Disease is medically correct.
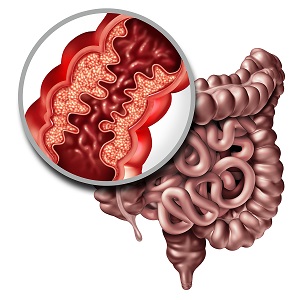
Could Crohn’s disease and Irritable Bowel Syndrome (IBS) really be caused by chronic intestinal yeast or fungal pathogenesis? Equally important is how these other fungal initiators of disease gain entry to the body? In most cases, they enter through the mouth from contaminated foods. Soon after, they often become activated from antibiotics, steroids, and other modern drugs that destroy the healthy stomach bacteria.
Once they get a hold on the digestive system yeast and their mycotoxins penetrate the lining of the stomach, cause inflammation in the intestinal lining, massive lesions like ulcers, and there’s no turning back. What’s more, the typical western diet continues to feed them their favorite food, which of course supports them in growing and spreading throughout your body. It is very common to have bloating, belching, intestinal gas, constipation, diarrhea, indigestion, and acid reflux as some common symptoms. What do you expect to happen once these microbial enemies pierce the lining of the stomach and enter the blood stream? Can they be stopped from wandering anywhere in your body?
Yeast Infections and Crohn's Disease
The common symptoms of crohns disease may include, diarrhea, abdominal cramps, rectal bleeding, weight loss, fever, and of course all other symptoms of a digestive systemic yeast infection. Additional symptoms may also include disorders of the eyes, liver, gallbladder, muscles and joints, kidneys, and skin. (Journal of Musculoskeletal Medicine Nov. 1996)
- (The Lancet 1996) Dr. Wakefield and colleagues found a direct link between a measles-infected mother during her pregnancy and development of Crohn’s disease in 3 out of 4 siblings later in life. Antibiotic resistant pneumonia preceded the disease in every case.
- Two of three worldwide studies found the average intake of carbohydrates (including bread, potatoes, and refined sugars) to be much greater in those that developed Crohn's. (Inflammatory Bowel Diseases 1990)
- Dr. A.V. Constantini (retired doctor working with the World Health Organization) found people with
Crohn's disease commonly have aflatoxin, which is a fungal carcinogenic mycotoxin in their blood.
- C.C.Kibbler, in 1996 describes how Blastomyces dermatitidis, a fungus, can produce lesions in the intestines. These types of lesions have been seen in patients with Crohn’s disease. The Histoplasma fungus produces intestinal disease histoplasmosis with symptoms such as diarrhea, weight loss, fever, and abdominal pain. The lesions that are seen in the intestines produce masses or ulcers mimicking IBS or carcinoma.
- A 2016 studythat was published in the Journal of Crohn’s and Colitis found a definite link to intestinal yeast and fungi to Crohn’s disease. They found that there was an overall reduction in the bacterial biodiversity with Proteobacteria and Fusobacteria at increased levels. Basidiomycota, Ascomycota, Cystofilobasidiaceae family and Candida glabrata fungal species were over represented in Crohn's disease patients.
Not surprisingly these two intestine - affecting diseases are most prevalent in the United States; which is more than likely due to the high amount of processed foods in our diet and the use and over prescribing of antibiotics.
Many existing studies indicate that indeed antibiotics, chemotherapeutic agents, steroids, and corticosteroids can significantly reduce normal intestinal bacteria levels, allowing the fungi to attach to the mucus lining of the intestines in immuno suppressed individuals.
Who are the immuno suppressed group of people? Scientists have shown that immune functions and strength has declined by 25% in adults as compared to 1960. Meanwhile, our farmland soils are now 85% depleted of nutrients that are required for maintaining a healthy diet. (1992 World Earth Summit) These nutrients cannot be absorbed in the plants or the vegetative flora if it is not in the soil.
The fungal species that can be involved are Candida albicans, and Candida tropicalis are the most prevalent species that infect the gastrointestinal tract as well as the entire human body. However, in 2016, a report pointed out that Candida glabrata is over represented in Crohn’s disease patients.
It is possible that Blastomyces dermatitidis, Coccidioides immitis, Histoplasma capsulatum, and Paracoccidioides brasiliensis can infect the digestive system and can be ascribed to Crohn’s disease and IBS mimicking their symptoms?
When it gets to the point of such a debilitating disease can also enter other organs - the liver, spleen, and lungs being the first targets. From there these fungal agents, especially the Candida species, possess the capability to get into every organ in the system. Unfortunately, most of the times these systemic yeast infections remain undiagnosed till the time an autopsy is conducted.
One thing is clear; when Candida yeast gets to the point of causing Crohn’s or irritable bowel syndrome symptoms, every single patient has been recorded to have a deficient or weakened immune system deficient in one way or another.
If you suffer from any of these two diseases I think it would be worth your time and effort go on the Diet recommended on this website and try a few proven supplements for at least a month. If you feel better and your symptoms are improved, then it is safe to assume you have found the cause of your illness as an intestinal yeast infection. Then you can take the necessary steps in your life to get rid of it or keep it at bay, much like a diabetic.
Dr. Atmika Paudel, PhD says...
Inflammatory Bowel Disease (IBD), including Crohn’s disease, has been linked with fungal infection of the gastrointestinal tract. With the recent advancements in the field of next-generation sequencing and metagenomic analyses, it has been more evident than before that these digestive tract illnesses have a close relationship with the fungal population present inside the gut (1). In a paper published in Gut journal, analysis of fecal samples from patients with inflammatory bowel diseases revealed that the relative ratios of pathogenic yeasts, including Candida albicans, were higher than healthy individuals (2). In another study, a similar phenomenon was observed where Candida glabrata species were highly present in the intestine of patients with Crohn’s disease (3). It is evident that the diet we consume directly affects the intestinal microbiota. A diet most commonly consumed in Western societies, in addition to antibiotics use, increases the colonization of Candida albicans in the intestine (4).
- Miyoshi et al., The evidence for fungus in Crohn's disease pathogenesis, Clinical Rev., 11:449-456, 2018. https://link.springer.com/article/10.1007/s12328-018-0886-9
- Sokol et al. Fungal microbiota dysbiosis in IBD. Gut, 66:1039–48, 2017. https://gut.bmj.com/content/66/6/1039.short
- Liguori et al. Fungal Dysbiosis in Mucosa-associated Microbiota of Crohn’s Disease Patients. J Crohns Colitis, 10:296–305, 2016. https://academic.oup.com/ecco-jcc/article/10/3/296/2462491?login=true.
- Mishra, et al., Adaptation of Candida albicans during gastrointestinal tract colonization Curr Clin Microbiol Rep, 5: 165-172, 2018. https://link.springer.com/article/10.1007/s40588-018-0096-8
Medical Review by Dr. Vibhuti Rana, PhD
A comprehensive review published by Stamatiades et al in 2018 discusses about all the available evidence suggesting the role of fungal infections in patients suffering from IBD. (1) This study also shows that the respiratory tract and the GI tract are most affected sites, especially in IBD patients undergoing anti-TNF alpha agents. Prof. Chris Probert from University of Liverpool says that the percentage of antibodies against some fungi is substantially higher in patients with Crohn’s as compared to those without the disease. (2) Similarly, chemical markers specific for fungi were also found in the stools of the Crohn’s patients and not the healthy controls. He concluded that the western diet tends to contain a large amount of yeasts, especially Saccharomyces and Candida, found to trigger inflammation in mice. This was simultaneously accompanied by a decline in the good bacteria Faecalibacterium.
Another study conducted over a period of 7 years across 10 European countries by a group of doctors led by Dr. Andrew R. Hart, MD, says that the role of diet in the etiology of IBD is plausible. (3) Western diet rich in yeast, sugar, and carbohydrates has been shown to cause dysbiosis and further lead to IBD in mice. (4)
1. Stamatiades GA, Ioannou P, Petrikkos
G, Tsioutis C. Fungal infections in patients with inflammatory bowel
disease: A systematic review. Mycoses. 2018;61(6):366–376. doi:10.1111/myc.12753.
2.
Examination of the fungal microbiome in Crohn’s disease and an
investigation of the impact of fungi on bacterial microbiota and their
interaction with phagocytic leucocytes. Professor Chris Probert,
Institute of Translational Medicine, University of Liverpool. 2015
3.
Chan SS, Luben R, van Schaik F, et al. Carbohydrate intake in the
etiology of Crohn's disease and ulcerative colitis. Inflamm Bowel Dis. 2014;20(11):2013–2021. doi:10.1097/MIB.0000000000000168.
4.
Martinez-Medina M, Denizot J, Dreux N, et al. Western diet induces
dysbiosis with increased E. coli in CEABAC10 mice, alters host barrier
function favouring AIEC colonisation. Gut. 2014;63:116–124.
Have Any Questions About Crohns Disease or IBS?
Do you have any questions about Crohns disease, IBS, or yeast infections in general? Ask your question here or contact us using the contact page of this website. It is also always a good idea to talk to your doctor as well.
Questions From Other Visitors
Click below to see questions from other visitors to this page...
Can Alkala-N taken as suggested cause diarrhea? 




I've cured my long term (15 years or so) IBS(?) with a very complicated recipe of top probiotics combined with many different kinds of fiber. It was recommended …
Systemic Yeast Infections and Crohns Disease Home Click Here
Article References
J Crohns Colitis. 2016 Mar;10(3):296-305. doi: 10.1093/ecco-jcc/jjv209. Epub 2015 Nov 15. Fungal Dysbiosis in Mucosa-associated Microbiota of Crohn's Disease Patients.
Home Privacy Policy Copyright Policy Disclosure Policy Doctors Store
Copyright © 2003 - 2025. All Rights Reserved under USC Title 17. Do not copy
content from the pages of this website without our expressed written consent.
To do so is Plagiarism, Not Fair Use, is Illegal, and a violation of the
The Digital Millennium Copyright Act of 1998.