- Home
- Species & Infections
- Candida Albicans
Candida albicans - What is It? How Do You Get It? How to Treat It
Updated 10/14/2021
Medically reviewed by Dr. Atmika Paudel, PhD - Written by Dr. Vibhuti Rana, PhD and Dan Jackowiak Nc, HHP
Dr. Atmika Paudel, PhD says... The facts and the information presented in this page about what Candida albicans is, how you get it and methods to get it under control are medically accurate.
Candida albicans is a type of fungal yeast with a predominately unicellular mode of development. It is responsible for a little over half of the fungal yeast infections in the United States and two thirds worldwide. The genus Candida as a whole comprises more than 150 species.
Candida reproduces by budding from a chain of connected spores called blastospores. Blastospores can be elongated, ovoid, or spherical although Candida albicans tends to have elongated ones, called pseudohypha, with lateral out growths of blastospores forming off the pseudohypha. It can be either white or an opaque light grey in color.
The cell is made up of 20-40% proteins, 30-50% polysaccharides, and varying proportions of lipids. These phospholipids are composed of phosphatidylcholine, phosphatidylethanolamine, phosphatidylserine, and phosphatidylinositol. Ergosterol is the predominant sterol although the amount of ergosterol varies from one subtype to another. The predominant fatty acids are oleic, linoleic, palmitic, and palmitoleic.
The cell wall runs three to five layers thick depending upon the yeast strain. The outer layer is mostly fibrillar with mannoproteins and can be compared to a capsule or coating. Mannan polysaccharide is found throughout the cell wall structure and forms the second and third layers. Layer four is mostly D-glucose derived glucans and the innermost layer is rich in chitin (a type of cellulose) and glucans. Chitin and glucans render rigidity to the cell much like the plant cell wall. Lipids are located throughout the layers. The cell has a plasma membrane and mitochondria for energy production.
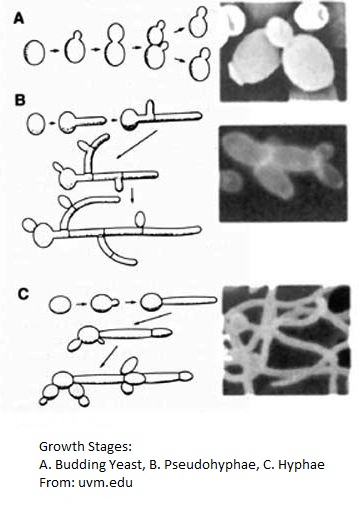
Like all pathogenic yeasts, Candida albicans builds a biofilm over itself as a means of protection from the host immune system. These biofilms contain pseudohypha with budding blastospores that are released from the biofilm as a way to colonize, further infecting the host. The more mature the biofilm, the more is the resistance to both prescribed anti-fungals and natural anti-fungals.
Its intracellular pH runs from 6.7 to 6.8, though mature hyphae have a pH of 6.4. It can survive in a pH range of 2.5 to 8.0 and thrives at a temperature range of 68°F to 103°F. When exposed to a pH under 6 (acidic environment), it grows in a yeast form. When exposed to a pH over 7 (alkaline environment), it shifts to a hyphal pathogenic form. Studies have suggested that 98.6°F is the optimal temperature for its growth.1
The vagina's pH is normally acidic (pH: 4), so Candida albicans will mostly exist in this environment in the spore form. However, it is has been medically proven that a vaginal pH around 4.5 or higher is a risk factor for yeast infections and bad bacterial overgrowth, known as bacterial vaginosis or BV.
The lumen of the stomach typically has a pH value of 2.0, because of which the yeast cannot survive there. The small intestine runs a pH of 5.7 to 7.4 to the ileum. The beginning of the colon is about 5.7 and it rises to 6.7 at the rectum. So for the most part, except in the lower small intestine, Candida albicans exists in the intestines as a spore form which typically causes no harm. However, if you alter the good bacteria in your gut, the ordinarily maintained pH rises, shifting the spore form to the pathogenic hyphal form. However, typically upon coming in contact with a surface it switches to hyphal growth.
Now, this is very important: In 2011, Vylkova et al. from the University of Texas Health Science Center discovered that Candida albicans has the ability to actively alkalize its surrounding environment under nutrient starvation.(2) This means that a nutrient deprived condition (no food), it raises the pH in the surrounding area and this induces hyphael formation! So following a candida diet that cuts All carbs is going to lead to a more severe infection!
In 1987, CE Webster and FC Odds discovered that C. albicans is aerobic and can double its population every two hours when oxygen is plentiful. This was confirmed by doctors S. Anand and R. Prasad from the Jawaharlal Nehru University, India in 1991 in their book entitled Candida Albicans: Cellular and Molecular Biology. They also found that under anaerobic conditions, it takes 20 hours to double its population. This was verified in 2004 by scientists Raluca Dumitru and Jacob M. Hornby with the Biological Sciences research unit at the University of Nebraska.
It secretes protease, phospholipase and lipase enzymes into the substrate it is attached to as a feeding mechanism. The broken down substrate will release glucose which is then sucked up like roots on a tree sucking water.
Candida albicans prefers carbohydrates and does require biotin for growth. In addition to biotin, thiamine, pantothenate, nicotinic acid, p-aminobenzoic acid and vitamin B12 also have a stimulatory growth effect. Carbohydrates can include other forms of sugar like sugar alcohols, milk sugar (lactose), and fruit sugar (fructose). However, a study done at Shiraz University of Medical Sciences in 1975 found that xylitol suppressed the growth of three different strains of C. albicans.
It also needs iron, zinc, copper and manganese, in that order of importance, for growth. As a matter of fact, a mild zinc deficiency has been associated with recurrent vulvovaginal candidiasis in women. Supplementing with zinc has been shown to reduce the incidence of candida infection in China. Restriction of zinc specifically led to the formation of enlarged, spherical yeasts, a phenotype term as Goliath cells.
In 1969, it was found that Candida albicans polysaccharides actually had antitumor activity against mouse sarcomas. Further investigation by Bistoni and associates have shown it is the glucan fraction that posses this tumour suppressive activity. The glucan stimulates neutrophil and macrophage activity. The same effect was observed with the glucans found in Saccharomyces cerevisiae, a type of Baker’s yeast. Most β Glucan products on the market today are made from these glucans.
Dr. Vibhuti Rana, PhD says…
Candida
spp.
has the ability to grow in extremely and diverse environments in
context to the availability of nutrients, temperature variation, pH,
osmolarity, and amount of available oxygen. (1) Candida
biofilms are very versatile and flexible in nature, and grow rapidly.
This is the reason that anti fungal drugs like Diflucan does not work
after some time. The Candida biofilm typically contains cellulosic plant matter, polynucleotides (DNA and RNA), polypeptide proteins, and
polysaccharide carbohydrate glucans, and lipids.
It has been shown that the growth of C. albicans in acidic environments enhances the sensitivity towards β-glucanase compared to a pH=6 or pH=8 grown cells. The yeast grows into a virulent form by hyphal expansion by apparently releasing ammonia and driving pathogenicity in the host. (3) This indicates that β-glucans are more accessible in cells grown in media buffered to pH=4. (2) Numerous reports have also stated the role of yeast glucans in suppressing tumors, as it can modulate the tumor microenvironment. (4,5).
1. de Oliveira Santos GC, Vasconcelos CC, Lopes AJO, et al. Candida Infections and Therapeutic Strategies: Mechanisms of Action for Traditional and Alternative Agents. Front Microbiol. 2018;9:1351. Published 2018 Jul 3. doi:10.3389/fmicb.2018.01351.
2. Sherrington SL, Sorsby E, Mahtey N, et al. Adaptation of Candida albicans to environmental pH induces cell wall remodelling and enhances innate immune recognition. PLoS Pathog. 2017;13(5):e1006403. Published 2017 May 22. doi:10.1371/journal.ppat.1006403.
3. Fernandes TR, Segorbe D, Prusky D, Di Pietro A (2017) How alkalinization drives fungal pathogenicity. PLoS Pathog 13(11): e1006621.
4. Chan GC, Chan WK, Sze DM. The effects of beta-glucan on human immune and cancer cells. J Hematol Oncol. 2009;2:25. Published 2009 Jun 10. doi:10.1186/1756-8722-2-25.
5. Geller A, Shrestha R, Yan J. Yeast-Derived β-Glucan in Cancer: Novel Uses of a Traditional Therapeutic. Int J Mol Sci. 2019;20(15):3618. Published 2019 Jul 24. doi:10.3390/ijms20153618.
How Do You Get Candida albicans?
It is believed that everyone has Candida yeast existing as a part of their microbiome in their gut. This microbiome is passed on to a baby when it is passing through the mother’s vaginal canal during the process of childbirth. There you are bathed in all the bacteria and yeasts that she has. Basically, you swallow these fluids and acquire her microbiome. Throughout life you will be exposed to more bacteria from your environment, including yeasts.
A normal microbiome is composed of 85% beneficial bacteria and 15% pathogenic microbes. This 15% will be composed of different species of bad bacteria and yeasts. The yeast level will be quite low and if the person maintains a healthy lifestyle, a proper diet, never takes antibiotics, and their immune system is strong, yeast and these pathogenic bacteria will never cause problems. However, in the real world, this is pretty much impossible!
People with HIV, compromised immune systems, diabetes, cancer patients, and those who use antibiotics or steroids often are usually most affected by C. albicans overgrowth. Patients in the intensive care units can also acquire infections from catheters as yeasts can grow on plastics.
In 2002, Francis A. Colardyn, MD, and his team of doctors determined that the mortality rate from blood stream infections runs about 34%, and can be as high as 78% if not treated within 48 hours. It has the ability to affect any organ in the body, shutting it down which results in death.
Compromised immune systems, central venous catheters, broad spectrum antibiotic use, trauma, intestinal surgery, and damage to the intestinal tract are the risk factors that account for systemic Candida yeast infections.
I go into great detail on all the typical causes of candida yeast over growth on this webpage.
Dr. Vibhuti Rana, PhD says…
The first thing to mention here is the tolerance level of your immune system. A study conducted by Kabir and Ahmad in 2012 clearly states that there has been a dramatic rise in the yeast infections worldwide, owing to the increase in immunocompromised patients.(7) They also say that whatever be the cause of yeast infection, all the treatment outcomes depend upon the early diagnosis of the infection and timely speciation of the Candida species. This opportunistic organism, if invasive, can even be fatal, damaging all the internal organs.
The five main species, existing in healthy human body are C. albicans, C. glabrata, C. tropicalis, C. parapsilosis, and C. krusei. They cause more than 90% of yeast invasive infections. (8) Unfortunately, Candida spp. Infection can even be picked up by immuno-suppressed patients in hospitals. A recent study conducted by de Oliveira Santos GC and team reported that Candidemia is the most frequent nosocomial (hospital-associated) infection with more that 49% mortality in immunocompromised patients. (9)
7. Kabir MA, Ahmad Z. Candida infections and their prevention. ISRN Prev Med. 2012;2013:763628. Published 2012 Nov 4. doi:10.5402/2013/763628.
8. Spampinato C, Leonardi D. Candida infections, causes, targets, and resistance mechanisms: traditional and alternative antifungal agents. Biomed Res Int. 2013;2013:204237. doi:10.1155/2013/204237.
9. de Oliveira Santos GC, Vasconcelos CC, Lopes AJO, et al. Candida Infections and Therapeutic Strategies: Mechanisms of Action for Traditional and Alternative Agents. Front Microbiol. 2018;9:1351. Published 2018 Jul 3. doi:10.3389/fmicb.2018.01351
Diagnosing Candida Albicans
Please check the symptoms and tests pages if you suspect that you have a candida albicans infection and want to verify.
How to Treat Candida albicans
The drug of choice is Fluconazole which is marketed as Diflucan in the United States. In the cases of vaginal yeast infection caused by Candida albicans, most doctors prescribe one or two pills as treatment. Deep rooted cases, however, can take up to six months to get under control.
It is possible, and I do see it all the time, for the yeast to become resistant to the point that Fluconazole does nothing. In these cases, Itraconazole, Voriconazole, Posaconazole, one of the Enchinocandins, and Amphotericin B are the suggested alternatives.
From a natural perspective there are quite a few things you can do. It is usually best to do all of them, which also tends to correct the underlying cause to start with.
Because we know now that all types of Candida albicans use glucose as their preferred source of carbon for growth, it is best to follow the right diet and don't cut off all carbs.
We are also aware now that it builds a biofilm over itself as a means of protection and as a method to expand within its host. Therefore, we have to have something that removes the biofilm. A properly designed enzyme formula will do this, and it will also eat the Candida itself.
The enzymatic compositions of many herbs have Candida killing abilities and should be taken in order to strip off the biofilm. I have a list of recommended herbs on this webpage.
More than likely, the main cause of the infection is a reduction in the 85% good bacteria population in the gut, restoring those populations is imperative for long term recovery. A properly designed probiotic with bacteria that actually work for Candida can help, simultaneously removing the excessive Candida yeast.
Then, it takes time... The body can heal itself and come back into balance but if it has taken years to get to where you are now, it is going to take a while to recover. For instance, if you have a long history of antibiotic or steroid usage and one of those antibiotics was a broad spectrum type, studies have shown it can take a year for your good bacteria to come back. Other non-broad spectrum antibiotics take three to six months to recover from.
To learn how to treat Candida albicans naturally click here.
Dr. Vibhuti Rana, PhD says…
An article published in Clinical Infectious Diseases in January 2004 emphasizes that yeast that cause such a broad range of infections (mild skin infections to fatal invasive ones) ought to be treated with an equally broad combination of therapies and diagnostics. Currently, Candida infected patients are commonly being treated with an assortment of antifungal medicines such as fluconazole, amphotericin B, nystatin, and flucytosine. (10) It has also been reported by Scott E. Evans of University of Texas M. D. Anderson Cancer Center that patients with HIV or other immunocompromising health conditions exhibit lower incidence of invasive candidiasis than do patients with cancer. (11) The timely and accurate diagnosis of infecting yeast is a serious issue. Often, it takes several days to obtain antifungal susceptibility information for Candida species, thus delaying the therapeutic applications (12)
As
far as the recovery of the healthy microbiota is concerned, it is not
an easy process. Candida possesses the unique properties of switching
their morphology, and therefore, has lower susceptibility towards the
treatment. (13)
Using correctly composed probiotics are very necessary to allow quick
and efficient treatment of such yeast infections. Among natural
remedies, use of tea tree oil and yoghurt, which is rich is
Lactobacilli,
also helps in restoring the dysbiosis. (14).
10. Peter G. Pappas, John H. Rex, Jack D. Sobel, Scott G. Filler, William E. Dismukes, Thomas J. Walsh, John E. Edwards, Guidelines for Treatment of Candidiasis, Clinical Infectious Diseases, Volume 38, Issue 2, 15 January 2004, Pages 161–189, https://doi.org/10.1086/380796.
11. Scott E. Evans. Coping with Candida Infections. 2010 May;7(3):197-203. doi: 10.1513/pats.200907-075AL.
12. de Oliveira Santos GC, Vasconcelos CC, Lopes AJO, et al. Candida Infections and Therapeutic Strategies: Mechanisms of Action for Traditional and Alternative Agents. Front Microbiol. 2018;9:1351. Published 2018 Jul 3. doi:10.3389/fmicb.2018.01351.
13. Tsui C, Kong EF, Jabra-Rizk MA. Pathogenesis of Candida albicans biofilm. Pathog Dis. 2016;74(4):ftw018. doi:10.1093/femspd/ftw018.
14. https://www.medicalnewstoday.com/articles/321342.php#home-remedies
Medical Review by Dr. Atmika Paudel, PhD
Candida albicans have the ability to change their form from yeast to hyphae, and this switch plays an important role in the survival of the fungi inside the host. Depending upon the environment and opportunity available, C. albicans reside in the body as a commensal or infects as a pathogen. The structure of the Candida cells and their brief reproduction pattern has been explained in the above article. At first, it was thought that C. albicans reproduced asexually, but later it was found that they do have sexual reproduction (1). More detail about candida cell structure and biofilm structure is also available on this page.
The biofilm of C. albicans is highly structured, encasing all the three forms of Candida cells- budding-type, pseudohyphae-type and hyphae-type cells inside an extracellular matrix. Biofilms can be formed inside the body or outside the body in medical appliances which is one of the leading causes of hospital-acquired C. albicans infections. Getting rid of Candida infections by using antifungals will cure the infections but on the other hand, antifungal agents have more side effects, this is because both fungi and human are eukaryotes, so selective specificity toward fungi is difficult to achieve and we have to weigh the pros and cons of the use of antifungals. Therefore, getting rid of fungi the natural way looks more beneficial to the body, where we boost the immunity, starve the fungi while getting enough nutrition for ourselves. Including proteins and fatty acids in the diet rather than carbohydrates will decrease Candida colonization in the human gut (2).
(1) Meleah et al., The ‘obligate diploid’ Candida albicans forms mating-competent haploids. Nature, 2013; DOI: 10.1038/nature11865.
(2) Hoffmann et al., Archea and fungi of the human gut microbiome: correlations with diet and bacterial residents, PlosOne, 8, e66019, 2013.
Any questions about Candida albicans or yeast in general, please feel free to contact us using the contact form on this website or talk to your doctor.
Main Article References
1.
A Watson in 1976, J. Bacteriol; M Lopez and C Silva in 1984, Z. Allg.
Mikrobiol 24; V. Uden and H. Buckley in 1970, The Yeasts; Lemos-Carolino
and Madeira-Lopes in 1984, Sabouraudia 22.
2.
MBio. 2011 May 17, Print 2011. The fungal pathogen Candida albicans
autoinduces hyphal morphogenesis by raising extracellular pH. Vylkova
S1, Carman AJ, Danhof HA, Collette JR, Zhou H, Lorenz MC.
3. Iralu, Appl. Microbial 22, 1971 and CE Webster, FC Odds J. Med. Vet. Mycol. 25, 1987.
Home Privacy Policy Copyright Policy Disclosure Policy Doctors Store
Copyright © 2003 - 2025. All Rights Reserved under USC Title 17. Do not copy
content from the pages of this website without our expressed written consent.
To do so is Plagiarism, Not Fair Use, is Illegal, and a violation of the
The Digital Millennium Copyright Act of 1998.