- Home
- Species & Infections
- Tinea
Tinea - The Cause of Most Fungal Skin Infections
Updated 05/11/2024
Written by Molecular Biologist Dr. Vibhuti Rana, PhD
Tinea infections are a group of fungal infections of the skin that may not be serious, but involve a lot of discomfort and unease. They are transmissible by touch, and may result due to dampness, or little exposure of skin surface to air and sun. One may also catch this infection by infected pets.
A few symptoms are a hallmark of tinea induced dermatitis- redness, itchiness, irritation, burning, or loss of hair at the affected site. Fungi known as dermatophytes lead to tinea infections of skin, nails, or hair (1). Dermatophytic fungi like Microsporum and Trichophyton species operate by adhering to skin cells, or keratinocytes and secreting various protease enzymes for invasion (2).
Immunocompromised individuals possess a higher risk of contracting tinea infections. Studies discuss that molecular make up of your genes also affect your susceptibility towards these infections. For instance, people with low defensin β 4 (DEFB4) copy number are predisposed to attack by tinea-causing dermatophytes (3). Besides, with age, a person’s immune system starts losing its power, metabolic diseases like diabetes come into play, longer exposure to pathogens occurs, and the blood circulation gets poor. What’s more, elderly people may feel difficulty in maintaining their skin, toe, nail, hair hygiene without external help. All these factors make them susceptible to skin, hair, or nail related tinea infections.
In this article, I will take you through the different kinds of tinea infections one can develop and their possible modes of treatment.
Different Kinds of Tinea Infections
There are many kinds of tinea infections based on their site of occurrence in body. Tinea capitis and Tinea corporis are more seen in pre-pubertal young children as compared to Tinea cruris, Tinea pedis, and Tinea unguium, that have a higher tendency of occurrence in adults (4).
Tinea capitis (scalp ringworm): Tinea capitis affects the scalp and may result in bald patches, dry areas in scalp, or redness. It can mainly be caused by Trichophyton or Microsporum species though the epidemiology differs in different regions of the world. It generally affects post 6 years of age in children or adolescent groups, and is most frequently observed in African American population (5). In this, the dermatophytes typically invade the hair shafts by secreting enzymes such as proteases that can even work in adverse acidic and alkaline environments (2).
Tinea pedis (Athlete’s Foot): It is a form of tinea infection that causes dryness, itching, burning, and cracked skin between one’s toes. It can even spread to the sole or sides of the feet and may be accompanied by presence of tiny painful vesicles or bullous tinea. The best that you can do to overcome this infection is to keep your feet dry, avoid closed shoes, use antifungal powders between toes and wash and dry your feet thoroughly after sweating (4). Since the favorite hiding spot for fungal spores are the insides of the shoes, we must take proper care to keep our shoes clean and dry. An old study in 1992 also suggested the use of tea tree oil-based creams/extracts to lessen the symptoms of Tinea pedis since it is a well-known anti-bacterial and anti-fungal natural compound. However, it was not as effective as the antifungal tolnaftate in patients (6).
Tinea
unguium (onychomycosis): This
is more of a cosmetic disease; a form of dermatophytic invasion of
fingernails and toenails that affects more than 10% of the US
population (7). Mostly, it is caused by Trichophyton
rubrum and is much harder to treat due to the
presence of hard nail plate of finger and toe nails and slow growth
of nails. Apart from rendering creating a cosmetic disadvantage and
inferiority complex in the affected people, its treatment takes a
toll on the pocket too.
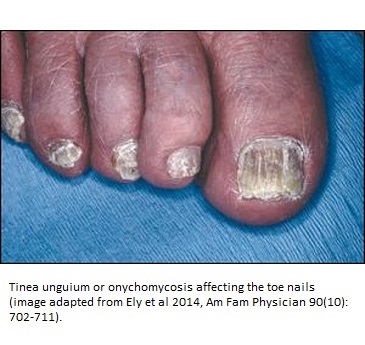
This transferable infection is more prone in immunocompromised individuals like those suffering from HIV, in aging population, and individuals performing high levels of fitness related activities (8). Reports also say that it may occur parallel to Tinea pedis and may run in the family. In children, this disease has not been given due importance and gets mistaken for other forms of toenail infections (9). Since children have thinner nails, topical antifungal therapy would work better than adults and is a promising field of research in pediatric groups.
Tinea corporis (ring worm)- Like Tinea capitis, this form of transferable dermatophytosis is also caused by Trichophyton and Microsporum species. It mainly affects the arms, trunks, or legs, though it may develop anywhere on the body. According to MSD Manuals, the drugs that are effective in eradicating Tinea corporis’s red ring-like, itchy patches on skin are terbinafine, imidazole, ciclopirox, and naftifine local ointments or creams (11).

Tinea corporis or ringworm can be mistaken for other diseases like psoriasis, eczema, or seborrheic dermatitis, which occur completely due to different etiological agents. In 1989, a very informative study by Summerbell et al reported that many other etiological species other than dermatophytes and yeasts contributed to nail, hair, and skin infections. These were identified as Scopulariopsis brevicaulis, Hendersonula toruloidea, and Aspergillus sydowii (12).
Tinea versicolor- This involves severe discoloration (pink, white, tan) or loss of melanin pigmentation. Infected stratum corneum and scaly epidermis are the key features of this disease. It mainly affects the neck, trunk or the shoulder area. Etiological agent is the infectious, hyphal form of the fungus Pityrosporum orbiculare or Malassezia (1).
A number of other tinea infections, that are not very frequent, include Tinea manuum (hands), Tinea faciale (face) and Tinea barbae (beard) (1, 13).
Once the fungal cells reach the host cells via skin, they go for adherence to the skin cells or keratocytes. Then they penetrate into the cells by releasing lytic enzymes like proteases, serine subtilins, and fungolysin. These molecules breakdown the detailed network of keratoycytes into small protein peptides or amino acids (13). They also impair the human immune response by mannan-induced inhibition of lymphocytes. They reduce the levels of IL-17 and IL-22, that are the most important immune cytokines which help in clearing the fungal infections.
How to Diagnose and Treat Tinea
Most of the Tinea cases can be identified based on their visual appearance, such as Tinea cruris, Tinea corporis, and Tinea pedis. For a 100% surety in case of atypical appearance, cultures need to be done and identified microscopically, or by using potassium hydroxide preparation.
Tinea corporis, Tinea cruris, and Tinea pedis generally respond to inexpensive topical agents such as terbinafine cream or butenafine cream, but oral antifungal agents may be prescribed for extensive disease, failed topical treatment, immunocompromised patients, or severe moccasin-type tinea pedis. Oral consumption of terbinafine constitutes the primary therapy for tinea capitis and tinea unguium because of its tolerability, high cure rate, and low cost. (4)
In case of Tinea capitis, even asymptomatic people may serve as carriers and be a source of infection. Mode of treatments that have been effective are terbinafine, itraconazole, fluconazole and griseofulvin (5). For Tinea corporis, imidazole, ciclopirox, naftifine, and terbinafine are used locally. Utmost care should be taken to continue applying the topical agents at the site of infection for a week even after the rash has disappeared (around three weeks) in order to avoid recurrence by leftover fungal spores (11).
Tinea corporis, Tinea cruris, and Tinea pedis respond to terbinafine and butenafine topical creams. Creams such as Lamisil-AT and Micatin AF are generally helpful and are available over the counter. However, in immunocompromised patients, extensive oral course may be required.
Other forms of Tinea like Tinea capitis, Tinea unguium, and chronic Tinea pedis are treatable only after oral antifungal usage and take longer times to cure. Some of these oral drugs are griseofulvin (Grispeg, Fulvicin), terbinafine (Lamisil), itraconazole (Sporonox), and fluconazole (Diflucan).
The pruritis caused by Tinea cruris can be treated with topical antimycotics like terbinafine, miconazole, clotrimazole, ketoconazole, econazole or usage of oral dozes of terbinafine and itraconazole for at least 2 weeks. Some patients may benefit from using anti dandruff medicated shampoos at the affected areas too (14).
It is highly advised to use the medicines for their complete recommended dosage religiously. In fact, no harm in continuing the medicines for an extra week or 10 days. Otherwise, the disease returns with an increased severity. The body areas prone to be infected must be kept dry and kept in sound hygienic conditions. Footwear sharing is strictly a NO and footwear should be cleaned periodically to eradicate the possibility of infection from the hidden fungal spores. Cotton garments should be preferred and too tight clothes aggravate the tinea conditions.
About the Author

Dr. Vibhuti Rana completed her Bachelors's Degree (Bioinformatics Hons.) from Punjab University and accomplished her Master’s Degree (2012) in Genomics with a Gold Medal from Madurai Kamaraj University, India. In 2020, she received her doctorate in Molecular Biology from the Council of Scientific and Industrial Research-Institute of Microbial Technology in affiliation with the Jawaharlal Nehru University, New Delhi, India.
Her focus areas include microbial drug resistance, epidemiology, and protein-protein interactions in infectious diseases. As a Molecular Biologist with extensive experience with infectious diseases, we are happy she is part of the YeastInfectionAdvisor team.
Back to Yeast Species and Infections
If you have any questions about tinea infections or about yeast infections in general, please feel free to contact us from the Contact page of this website or see your doctor.
Dr. Rana's Medical References
- Berger TG, TINEA INFECTION – AN ILLUSTRATED GUIDE 2014, British Journal of Family Medicine
- Hay, R.J. Tinea Capitis: Current Status. Mycopathologia182, 87–93 (2017). https://doi.org/10.1007/s11046-016-0058-8. https://link.springer.com/article/10.1007/s11046-016-0058-8
- Jaradat SW, Cubillos S, Krieg N, Lehmann K, Issa B, Piehler S, Wehner-Diab S, Hipler UC, Norgauer J. Low DEFB4 copy number and high systemic hBD-2 and IL-22 levels are associated with dermatophytosis. J Invest Dermatol. 2015 Mar;135(3):750-758. doi: 10.1038/jid.2014.369. Epub 2014 Sep 1. PMID: 25178103. https://pubmed.ncbi.nlm.nih.gov/25178103/
- Ely JW et al., Diagnosis and Management of Tinea Infections. 2014. Am Fam Physician. Nov 15;90(10):702-711. https://www.aafp.org/afp/2014/1115/p702.html
- A. K. Gupta, R. C. Summerbell, Tinea capitis, Medical Mycology, Volume 38, Issue 4, 2000, Pages 255–287, https://doi.org/10.1080/mmy.38.4.255.287. https://academic.oup.com/mmy/article/38/4/255/968935
- Tong MM, Altman PM, Barnetson RS. Tea tree oil in the treatment of tinea pedis. Australas J Dermatol. 1992;33(3):145-9. doi: 10.1111/j.1440-0960.1992.tb00103.x. PMID: 1303075. https://pubmed.ncbi.nlm.nih.gov/1303075/
- Elewski BE. Onychomycosis: pathogenesis, diagnosis, and management. Clin Microbiol Rev. 1998;11(3):415-429. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC88888/.
- Scher RK. Onychomycosis: a significant medical disorder. J Am Acad Dermatol. 1996 Sep;35(3 Pt 2):S2-5. doi: 10.1016/s0190-9622(96)90061-4. PMID: 8784302. https://pubmed.ncbi.nlm.nih.gov/8784302/
- Eichenfield LF, Friedlander SF. Pediatric Onychomycosis: The Emerging Role of Topical Therapy. J Drugs Dermatol. 2017 Feb 1;16(2):105-109. PMID: 28300851. https://pubmed.ncbi.nlm.nih.gov/28300851/
- https://www.merckmanuals.com/professional/dermatologic-disorders/fungal-skin-infections/tinea-cruris-jock-itch
- Aaron DM. Body ringworm (tinea corporis), 2020. MSD Manuals consumer version. https://www.msdmanuals.com/home/skin-disorders/fungal-skin-infections/body-ringworm-tinea-corporis
- Summerbell RC, Kane J, Krajden S. Onychomycosis, tinea pedis and tinea manuum caused by non-dermatophytic filamentous fungi. Mycoses. 1989 Dec;32(12):609-19. doi: 10.1111/j.1439-0507.1989.tb02192.x. PMID: 2533665.
- Sahoo AK, Mahajan R. Management of tinea corporis, tinea cruris, and tinea pedis: A comprehensive review. Indian Dermatol Online J. 2016;7(2):77-86. doi:10.4103/2229-5178.178099. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4804599/
- https://www.aocd.org/page/FungusInfections? American Osteopathic College of Dermatology.
Home Privacy Policy Copyright Policy Disclosure Policy Doctors Store
Copyright © 2003 - 2025. All Rights Reserved under USC Title 17. Do not copy
content from the pages of this website without our expressed written consent.
To do so is Plagiarism, Not Fair Use, is Illegal, and a violation of the
The Digital Millennium Copyright Act of 1998.