- Home
- Women's Infections
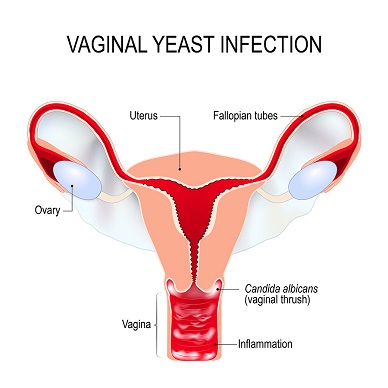
- Vaginal Yeast Infection
All About Vaginal Yeast Infection
Updated 10/06/2021
Medically reviewed by Dr. Atmika Paudel, PhD - Written by Dr. Shalaka Samant PhD and Dan Jackowiak Nc, HHP
Dr. Atmika Paudel, PhD who says... The information provided in this article about vaginal yeast infection - the causes, symptoms, and remedies for the same is medically correct.
Vaginal yeast infection is the most common women's yeast infection. Their causes, symptoms, and natural treatments without drugs, and the unwanted side effects are covered here. It is possible to eliminate many reoccurring infections in women, by treating the cause and not just the very uncomfortable effects.
According to experts, 75% of women will, by their mid 20's, experience a vaginal yeast infection. Half of those women will suffer through 4 or more infections a year.
Vaginal yeast infections in 2002 alone cost women over half a billion dollars on over the counter medications for this extremely common infection.
Dr. Shalaka Samant, PhD says...
Vaginal yeast infection is an inflammatory condition caused by yeast, primarily by the polymorphic opportunistic fungus Candida albicans. However, other Candida species might also sometimes be isolated as causative agents. Candida normally lives on the skin and inside the body, in places such as the mouth, throat, gut, and vagina, without causing any problems (1).
1. Vulvovaginal candidosis. Lancet. 2007 Jun 9;369(9577):1961-71.
Common Vaginal Yeast Infections Symptoms
Vaginal burning
Vaginal itching
Cottage cheesy discharge
Urinary disorders
Bladder infections
Recurring vaginitis
Menstrual irregularities
Worsening premenstrual syndrome
Burning during and after intercourse
Dr. Shalaka Samant, PhD says...
Sometimes Candida can multiply and cause an infection if the environment inside the vagina changes in a way that encourages its growth. This condition results in severe genital itching and soreness, vaginal odor, pain during sexual intercourse, pain or discomfort during urination, and abnormal discharge. Although most vaginal candidiasis is mild, some women can develop severe infections involving redness, swelling, and cracks in the wall of the vagina.
Widely available antifungals cure the condition however, about 15-20% of the women experience a repeat infection within 1 to 3 months. In addition, the high resistance levels in non-candida albicans species to the commonly used treatments associated with an increasing identification of these other species in patients underlines the importance of identifying Candida species within vaginal samples, in order to provide physicians with information concerning the proper treatment for their patients (2).
2. Bruna Gonçalves, Carina Ferreira, Carlos Tiago Alves, Mariana Henriques, Joana Azeredo & Sónia Silva (2016) Vulvovaginal candidiasis: Epidemiology, microbiology and risk factors, Critical Reviews in Microbiology, 42:6, 905-927, DOI: 10.3109/1040841X.2015.1091805
Typical Vaginal Yeast Infection Causes
These infections affect women with poorly controlled diabetes, immune system dysfunction, or women with immune deficiencies and they seem to be the most at risk for recurrent infections. Depressed immunity may occur as a result of nutritional deficiencies, medications, pregnancy, or serious illness. Scientists know that since 1960, immune function in adults has declined by 25%.
Immune Dysfunction
Many scientists believe that some women have some kind of t-cell lymphocyte problem that allows colonization by the mycelial form of candida in the vagina. Once established it begins to reproduce the spore form of candida, which has the ability to double its population every hour.
Dr. Shalaka Samant, PhD says...
Several
host-related
and behavioral risk factors
have been proposed as predisposing factors for vaginal yeast
infections (3). Host-related factors include pregnancy, hormone replacement,
uncontrolled diabetes, immunosuppression, antibiotics, glucocorticoids
use and genetic predispositions. Behavioral risk factors include use of
oral contraceptives, intrauterine device, spermicides and condoms and
some habits of hygiene, clothing and sexual practices.
3. Risk factors for recurrent
vulvovaginal candidiasis in women receiving maintenance antifungal
therapy: results of a prospective cohort study. Am J Obstet Gynecol. 2004 Mar;190(3):644-53.
It has also been proven that the normal vaginal flora is greatly altered in women with vaginal candida yeast and that many times candida can live right alongside L. acidophilus without any problems.
Many women have been found to have low zinc plasma levels, which reduces immune function. Some women have a defect in a prostaglandin secretion by the patient’s macrophages which blocks the proliferatory response of the lymphocytes that kill yeasts.
Other patients have decreased killing function by peripheral neutrophils and deficiencies in IgA secretory component in vaginal samples. IgA deficiencies are very common and the condition is usually for life but taking colostrum can help raise these levels. Excessive glucose levels are a problem and this can be secondary to low grade bacterial infection.
The immune system problems above have been clearly linked to estrogen dominance. In a scientific study done in 1999 by Paul L. Fidel Jr., Jessica Cutright, and Chad Steele of Louisiana State University, published in the American Society of Microbiology in 2000, found that progesterone had no effect on vaginal candida in mice but excess estrogen promoted it's growth. They also found that excess estrogen reduced the ability of skin cells, and the t-cells that protect them, to prevent colonization of candida on the vaginal walls.(1)
Elevated Estrogen Levels
Estrogen is also responsible for glycogen levels in the vagina and glycogen feeds yeast. An excess of estrogen has been linked to breast cancer and reduced function of the Thymic gland. The Thymic gland helps immune system t-cells that are grown in the bone marrow mature. At a certain stage of t-cell growth in the bone marrow they migrate to the thymic gland to complete this process. Upon maturity of the t-cells, the thymic gland releases them into the body.(2,3)
To find out if you might be estrogen dominant or have other hormone imbalances click here.
Dr. Shalaka Samant, PhD says...
Yeast vaginal infections could also have a hormone dependency. The walls of the vagina are lined with epithelial cells, which produce glycogen in proportion to hormonal levels. Elevated estrogen levels due to hormone replacement therapy, pregnancy, etc. stimulate the vaginal epithelium to produce glycogen, potentially facilitating the growth of Candida (4).
High estrogen levels are also thought to dampen the ability of vaginal epithelial cells to block Candida growth. Immunosuppressive conditions such as HIV-infection (5), cancer chemotherapy, glucocorticoids therapy (6), organ transplant, cancer, diabetes mellitus, tuberculosis, and any chronic debilitating illness can increase the chances of developing vaginal yeast infections.
4. Effects of Reproductive Hormones on Experimental Vaginal Candidiasis. Infect Immun. 2000 Feb; 68(2): 651–657.doi: 10.1128/iai.68.2.651-657.2000
5.
Incident and persistent vulvovaginal candidiasis among human
immunodeficiency virus-infected women: Risk factors and severity. Obstet
Gynecol. 2003 Mar;101(3):548-56.
6. Immunological aspects of cancer chemotherapy. Nature Reviews Immunology · February 2008.
Taking Antibiotics Recently
Taking antibiotics is a major cause of vaginal yeast infection as well as intestinal yeast infections. Most of the time the yeast has actually spread through the anus to the vagina. Rectal itching is the most common symptom that confirms this is indeed what is happening but this can also indicate parasite infestation.
Women who wear synthetic pantyhose a lot, have three times the yeast infection rate of women who wear cotton underwear, due to the fact cotton allows the natural vaginal secretions to dry and some synthetic materials do not.
Dr. Shalaka Samant, PhD says...
Vaginal
or systemic antibiotic use is often associated with incidence of vaginal
yeast infections. Antibiotic use leads to the depletion of the vaginal
bacterial microflora, which represents the dominant
vaginal defense
mechanism against Candida (7).
In addition, poor personal hygiene can increase Candida load. This infection can be also due to exogenous Candida acquisition through some sexual practices, including frequent sexual intercourse and receptive orogenital intercourse.
7. Microbiology of the female genital tract. American Journal of Obstetrics and Gynecology Volume 156, Issue 2, February 1987, Pages 491-495.Women are exposed to more chemicals than men due to commercially made cosmetics that contain mercury and lead, facial cleansers and moisturizers, body lotions, and perfumes. All these chemicals within these products gradually wear down the immune system allowing yeast to eventually take control, usually after some kind of illness. There are also xenoestrogens in many of these products that act like estrogen in the body.(4)
Too Much Yeast in the Intestine
The general consensus is that most recurrent cases of vaginal
yeast infection are due to the transmission from the gastrointestinal
tract and estrogen dominance. As a matter of fact, studies have shown
that 100% of women infected with chronic vaginal yeast also have it in
their intestine. Knowing this, it is best to treat the infection in the intestine while also treating the vaginal infection locally.
Sex With Infected Males
Up to 50% of people have yeast in their mouths so most sexually acquired infections are due to oral sex.(5) However, about 15% of men do have yeast growing on their penis so it is possible to become infected during intercourse.
Many women with non-chronic vaginal infections will have undetectable yeast levels in their stool, confirming that sex with an infected male is the cause of their vaginal yeast infection.
STD and Not Yeast
Quite often women mistake herpes or other STDs for a vaginal yeast infection. Check with your doctor to get tested or get it done directly here if you think this could be a possibility.
Some women actually misdiagnose bacterial vaginosis as a yeast infection, but the treatment is close to the same as far as safe and natural alternatives are concerned since they are caused by the same thing, a lack of good bacteria in the body.
Good Bacteria Overgrowth
Cytolitic vaginosis is also misdiagnosed as a yeast infection because it mimics the symptoms of vaginal yeast. Cytolytic vaginosis is also known as lactobacillus overgrowth syndrome or Doderlein's cytolysis. It can be easily identified by measuring vaginal pH and smell testing. If the vaginal discharge smells bad it is an overgrowth of Gardnerella, which is the most common bacteria that causes bacterial vaginosis. If it does not smell and the pH measures 3.5-4.5, cytolytic vaginosis is the problem.(6)
Treatment for Cytolytic vaginosis is simple and is directed towards reducing the number of Lactobacilli by elevating the vaginal pH. Treatment involves douching with sodium bicarbonate solution or using a sodium bicarbonate suppository vaginally. Douches are carried out twice weekly for every two weeks. Mix 1–2 tbls of baking soda with four cups of warm water. Alternatively, empty gelatin capsules are filled using baking soda and one capsule is inserted intravaginally, twice weekly for every two weeks. These measures help in resolving the symptoms by restoring the normal vaginal environment. If the symptoms persist or worsen beyond 2–3 weeks after initiating treatment, re-evaluation is required.
Dr. Shalaka Samant, PhD says...
In some patients who have symptoms and signs of vaginal candidiasis, which is unresponsive to antifungal drugs, a diagnosis of cytolytic vaginosis may have to be suspected. Cytolytic vaginosis is also known as lactobacillus overgrowth syndrome or Doderlein's cytolysis (8). It is characterized by abundant growth of Lactobacilli resulting in lysis of vaginal epithelial cells; and therefore, it is called as cytolytic vaginosis.
Accurate diagnosis and care to address the cause of vaginal yeast infections is therefore very important. The diagnosis of vaginal yeast infections requires correlation of clinical findings and laboratory confirmation of Candida.
8. Cytolytic vaginosis: misdiagnosed as candidal vaginitis. Infect Dis Obstet Gynecol. 2004; 12(1): 13–16.doi: 10.1080/10647440410001672139
How to Diagnose Vaginal Yeast Infection
If most of the symptoms I mentioned above apply to you then you probably do have vaginal yeast. If it also smells bad that is caused by bad bacteria and is called bacterial vaginosis. It is possible to have both at the same time.
Your gynecologist can take a swab and look at it under a microscope. If yeasts with hyphae are observed, you probably are infected with Candida albicans or a different hyphael producing yeast species.
If yeast with no hyphae are observed, you are probably infected with Candida glabrata. C. glabrata does not produce hyphae, only spores. It also does not produce the cottage cheesy discharge but does produce a clear discharge.
A swab sample can also be sent to a lab where they can run a culture to determine species or determine if the problem is Cytolic vaginosis. Knowing what species it is will allow your doctor to prescribe the correct drug for that yeast species.
Dr. Shalaka Samant, PhD says...
Since the symptoms of vaginal yeast infections are similar to those of other types of vaginal infections it is best to contact your healthcare provider to determine if it is indeed a yeast infection that is bothering you. Abnormal vaginal discharge can also point towards trichomoniasis and bacterial vaginosis (9).
9. Current evaluation and management of vulvovaginitis. Clin Obstet Gynecol. 1999 Jun;42(2):184-95.
Medicines Typically Taken for Vaginal Yeast Infection
Diflucan is the most popular prescribed drug for vaginal yeast infections, and most doctors usually prescribe one to three tablets thinking this will solve the problem. In milder infections it quite often does the trick.
Sometimes it doesn't because the yeast has spread and become too deeply ingrained in the tissues where it actually hides from the drug. The infection disappears but usually always seems to return in a short time. Continued use can cause an adaptation of Candida where other species like Candida glabrata take up residence, C. glabrata is more resistant to Diflucan because of the biofilm it creates to defend itself.
Miconazole in the form of a cream such as Monistat quite often works for mild vaginal yeast infections. Treatment times vary from one to seven days.
Clotrimazole also comes in a cream form and is used for seven days for milder infections.
There are also many natural vaginal yeast infection remedies that have been proven to work for these yeast infections.
The problem with all these common medications is they in no way shape or form treat the cause of vaginal yeast infection. Even powerful anti-fungals can be hit and miss since there is no way to determine when to stop taking these drugs without testing. This problem is compounded by the fact that fungi have the ability to build resistance to modern drugs like bad bacteria. All too often the yeast infection returns in a very short time, requiring more drugs. You continue on this vicious circle of relief, then flare up, not to mention some potentially dangerous side effects.
Medical Review by Dr. Atmika Paudel, PhD
The above article summarizes the major factors that are associated with the vaginal yeast infection, which are correct. It also briefly talks about common symptoms, how can we know if it is yeast infection, and ways to treat in an event of yeast infection.
As mentioned in the article above, a correct diagnosis at correct time would save women from recurrent yeast infection of the vagina. Diagnosis is very important in any disease, because treatment of the ailment greatly depends upon the diagnosis. If the diagnosis is correct, appropriate treatment would be provided and the disease will disappear. However, if misdiagnosis happens, then the medicines used would not work and people cannot get rid of the ailments easily, leading to further deterioration of the condition.
As we all know by now that imbalance of the normal microbiota of the vagina as well as intestine will lead to vaginal yeast infection. We will need to maintain the flora of good bacteria in our body. Indeed, lactobacilli recue the recurrence of vaginal yeast infection (1). However, as mentioned in the above article, some conditions such as cytolytic vaginosis is caused by the overgrowth of the lactobacilli, which are the so-called good bacteria. In an event of cytolytic vaginosis, the overgrown bacilli will start to damage the vaginal cells. In one of the studies, it was found that Lactobacillus crispatus had the ability to produce more acid in women with cytolytic vaginosis compared with the healthy women (2), suggesting that some host-factors and environment predispose women to cytolytic vaginosis.
Care should be taken when symptoms arise and appropriate diagnosis and treatment are the key to get rid of the infections, be it bacterial infection or yeast.
1. Ang XY, Chung FY, Lee BK, Azhar SNA, Sany S, Roslan NS, Ahmad N, Yusof SM, Abdullah N, Nik Ab Rahman NN, Abdul Wahid N, Deris ZZ, Oon CE, Wan Adnan WF, Liong MT. Lactobacilli Reduce Recurrences of Vaginal Candidiasis in Pregnant Women: A Randomized, Double-Blind, Placebo-Controlled Study. J Appl Microbiol. 2021 May 22. doi: 10.1111/jam.15158.
2. Yang S, Liu Y, Wang J, Li S, Zhang Y. Variation of the Vaginal Lactobacillus Microbiome in Cytolytic Vaginosis. J Low Genit Tract Dis. 2020 Oct;24(4):417-420. doi: 10.1097/LGT.0000000000000565.
Have Any Questions About Vaginal Yeast Infections?
Do you have any questions about vaginal yeast infection or yeast infections in general? Ask your question here or contact us using the contact page of this website. It is also always a good idea to talk to your doctor as well.
Questions From Other Visitors
Click below to see questions from other visitors to this page...
What treatment is best for vaginal or genital yeast infections? 




A female and husband have a vaginal yeast/genital infection. What meds are best for treatment???
Vaginal Yeast Infection Testimonials
hi Dan
I just wanted to leave a testimonial.
I had been a severe sufferer of yeast my entire life, my pain would get so severe that it would feel like I was on fire. Towards the end it became constant. I tried western medicine, I changed my diet...but nothing worked. I got sick and tired of doctors feeding me the same medicine with no result, and sometimes what they gave me actually made it worse. I did try acupuncture which helped, but did not clear my problem...
After finding you, I tried your suggestions. The Biofase and the Candidate worked amazingly. I also started to eliminate foods that have antibiotics and pesticides as much as possible. I also removed all chemicals from my home (cleaning products and body products) and only use natural/organic. I don't know if this helped, but I started to use a steam room once in a while...it did make me feel better.
It took about 3 months and I started to see huge results. Since then I
have been yeast free. If I ever feel a "tickle" I just go back on my
products and it disappears.
It is very difficult to explain to someone how this stops your entire
life..your marriage, your work, your mental and physical life...you are
unable to function..you are unable to enjoy life. Depression sets in
when you have pain in your body.
I have a great sex life now with my husband (I also want to thank my hubby for being there and loving me the entire time)...
I feel fantastic now...thank you!
Barbra
*****
Hi Dan,
I just returned from a visit with my GP. She did a vaginal exam, & there is NO yeast! She isn't quite sure what to think, since when she saw me last August, I had a significant yeast infection. And now, thanks to you!!! it's gone.
Talk soon,
THANKS!!!
Lynn
*****
Hi Dan,
Long time no speak..I wanted to let you know how things were going with me..I have been on the diet and pills for 1 month so far AND I HAVE LESS DISCHARGE! HARDLY ANY! I am so happy with your advice! I will be continuing to do the diet and take pills...just wondering if I am able to stay on the YST Management pills for a while? I seriously believe that they helped me a lot. Just wondering if I stay on them should I take it 2 times a day? or can I cut down to one? the diet has been going ok...I am introducing foods back into it..but am not taking any chances...cause I want this to be completely cleared....ok well thank you again
talk to u soon
Dana
I let Dana know she could stay at 2 a day indefinitely and to be careful with the processed grains and sugar. This is also the time to start re-introducing good bacteria into her body so this never recurs again. By the way, Dana had this problem for 5 years straight!
*****
Thanks Dan.
No longer suffer from Yeast infections.
Thanks for you help!
Carrie
*****
Hi Dan,
Thank you for this website, you have helped me a great deal. I have spent countless hours searching for an answer that doesn't lead to STD and end. I really appreciate that you pointed out how most doctors treat the symptoms but don't cure the problem. I think the world should be more aware of the true underlying causes of these infections instead of being pressured by the STD scare. No other site has provided me with an actual list of things to stay away from or such an extensive list of symptoms and their relations with the issue. I have been trying to link my problems and I couldn't find another site relating them at all but, inside I knew they had to be related. This has been THE MOST HELPFUL site EVER.
Thank You So Much for making this research as calming and thorough as it can get. I now know what tests to ask my doctor for, what foods to eat, and how to ease my suffering without resorting first to medications and creams that could make it worse. I thank you, my body thanks you, and my sex life definitely thanks you. Keep up the good work, it's inspiring.
Diane
*****Hello Dan,
Sincerely,
Vicky
Back to Womens Yeast Infections
Article References
1. Effects of Reproductive Hormones on Experimental Vaginal Candidiasis. Paul L. Fidel Jr., Jessica Cutright and Chad Steele. American Society of Microbiology 2000
2. J Clin Invest. 2016 Apr 1; 126(4): 1525–1537. Published online 2016 Mar 21. doi: 10.1172/JCI81894PMCID: PMC4811157Estrogen-mediated downregulation of AIRE influences sexual dimorphism in autoimmune diseases
3. Immunology. 2001 May; 103(1): 17–25. doi: 10.1046/j.1365-2567.2001.01212.xPMCID: PMC1783216. Role of oestrogen receptors α and β in immune organ development and in oestrogen-mediated effects on thymus.
4. Steroids. PMC 2008 Feb PMCID: PMC1862644NIHMSID: NIHMS19509. Xenoestrogens are potent activators of nongenomic estrogenic responses.
5. Geiger AM, Foxman B, Gillespie BW. The epidemiology of vulvovaginal candidiasis among university students. AM J Public Health 85:1146, 1995
6. Indian J Sex Transm Dis. 2009 Jan-Jun; 30(1): 48–50. doi: 10.4103/0253-7184.55490 PMCID: PMC3168042. Cytolytic vaginosis: A review.
Home Privacy Policy Copyright Policy Disclosure Policy Doctors Store
Copyright © 2003 - 2024. All Rights Reserved under USC Title 17. Do not copy
content from the pages of this website without our expressed written consent.
To do so is Plagiarism, Not Fair Use, is Illegal, and a violation of the
The Digital Millennium Copyright Act of 1998.