- Home
- Find the Cause
- Antibiotics Cause Yeast
Can Antibiotics Cause Yeast Infections?
Updated: 10/13/2021
Medically reviewed by Dr. Atmika Paudel, PhD - Written by Dan Jackowiak Nc, HHP and Dr. Vibhuti Rana, PhD
Antibiotics cause yeast infections because in addition to killing the bacteria that may be giving you an infection, they also kill the good bacteria that keep yeast under control.
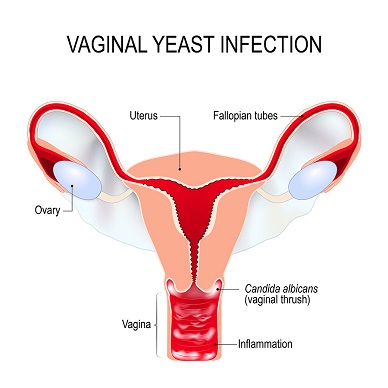
Normally, candida yeast lives in the vagina and intestines at very low levels, undetectable on stool tests or vaginal cultures. They are kept under control by your good bacteria but antibiotic anti-bacterial agents also kill these good bacteria, which can result in yeast getting out of control.
This page reviews what antibiotics are, how they cause yeast infections, if they can cause other other health problems, where they come from, what to do if you have to take them and what you should do if the antibiotics do cause a yeast infection.
What are Antibiotics?

According to Websters dictionary, "Biotic" means, relating to, or caused by living organisms, having a (specified) mode of life.
"Anti" means, one that is opposed or against.
So antibiotic means against life.
These substances are produced by one organism to kill/inhibit the growth of another organism. In fact, antifungal agents are also antibiotics.
They are typically made from substances that are produced by fungi or bacteria themselves, through a fermentation process. They can then be chemically enhanced in many cases.
Some antibiotics are made from chemicals, such as the quinolone class known as fluoroquinolones. Fluoroquinolones have broad spectrum anti-bacterial abilities and are cable of killing gram positive and gram negative bacteria. Ciproflaxin is a very commonly used broad spectrum antibiotic.
Plants
of all types also produce substances that could be considered
antibiotics. These substances will have natural antibiotic effects
against that plants natural fungal or bacterial predator.
For the purpose of this article, we are talking about antibiotics that are effective against bacteria.
Dr. Vibhuti Rana, PhD says...
It is by now understood that the change in the bacterial ratio in the gut and the vaginal surface leads to yeast infections. One of the most common types of vaginitis is yeast infection or Candidiasis. According to the data reports by the American College of Obstetricians and Gynecologists, it has been clearly stated that use of some kind of antibiotics changes the normal balance of the vagina and most frequently results in yeast infections (1). In a review published in 1966, Seelig has discussed that there is a huge impact of antibiotics like chlortetracycline on the severity of fungal infections in the alimentary canal by suppressing the host defense mechanisms (2).
1. American College of Obstetricians and Gynecologists
2. Seelig MS. Mechanisms by which antibiotics increase the incidence and severity of candidiasis and alter the immunological defenses. Bacteriol Rev. 1966;30 (2):442–459.
Why Do Antibiotics Cause Yeast Infections?
Most antibiotics, other than broad-spectrum types, are targeted to individual species of bacteria. So in theory, taking these antibiotics should not upset your good bacteria balance in your gut and vagina. But when put to use in the human body, they do, antibiotics kill both good and bad bacteria if the bacteria is susceptible to the antibiotic.
Basically, the antibiotic strips the good bacteria in your vagina that defends you from yeast. If enough good bacteria is stripped away, or killed, a vaginal yeast infection is the result.
Because you take these antibiotics by mouth, good bacteria levels in the intestine are also reduced, which could allow intestinal yeast to get out of control. If yeast does get out of control in the intestine, because of the proximity of the anus to the vagina, it can transfer. This process results in chronic vaginal yeast infections, month after month as as you re-infect yourself.
If you take to many antibiotics within a year, it can become a never-ending cycle. Many women will get an antibiotic for their cold or flu, urinary tract infection, etc and get a vaginal yeast infection as a result. The doctor gives them an anti-fungal or an anti-fungal cream, or they purchase it over the counter at the local drugstore. The infection may go away for a little while, but then it returns. This will continue to happen until the resulting antibiotic destruction to the microbiome has recovered.
These Medical Studies Prove Antibiotics Kill Good Bacteria
In 2000, in vivo experiments performed in mice and published in "Principals and Practices of Infectious Diseases", found a "single injection of streptomycin eradicated the protective effect of normal flora", which of course, could lead to an overgrowth of yeast.(Source) Streptomycin is usually prescribed for people that are allergic to penicillin.
In 2015, a study done by multiple doctors and scientists in the UK and Sweden, found that a single 10-day course of antibiotics in adults not only reduces the bacterial population but also reduces the overall diversity of the intestinal microbiome. Depending upon the antibiotic used, these effects lasted anywhere from three months for Amoxicillin, to a year, for a broad spectrum antibiotics such as Ciprofloxacin. The largest reduction has been recorded in the bacteria producing butyrate, which protects the intestine from inflammation and tumors.(Source)
A team lead by Dr. Ahmad Khan in India, demonstrated in 2009 that antibiotics, pregnancy, and contraceptives, all contributed to vaginal yeast infections. Antibiotics are prescribed most commonly for upper respiratory infections. However, according to Dr. Carol Kauffman from University of Michigan Medical School, "Most of these infections are caused by fungi". Even though these infections do not require any antibiotic treatment, doctors continue to prescribe them, ultimately altering the natural delicate balance of gut bacteria, allowing the yeast to overgrow and lead to a full-blown yeast infection.
Dr. Vibhuti Rana, PhD says...
Though antibiotics have done wonders to save millions of lives globally, they have molded the ecology of the microflora, resulting in altered consequences. Antibiotic usage harms the beneficial bacteria in human hosts (3). A study conducted at the Yonsei University College of Medicine, Korea illustrates that antibiotics give rise to altered intestinal microflora; with elevated number of bad bacteria due to exploitation of sugar, free radicals, and oxygen by them (4). The many symptoms of sepsis, treated by antimicrobials, result in this imbalance causing a long lasting effect on the microbiota which may never by completely recovered (5).
3. Langdon A, Crook N, Dantas G. The effects of antibiotics on the microbiome throughout development and alternative approaches for therapeutic modulation. Genome Med. 2016;8(1):39. Published 2016 Apr 13. doi:10.1186/s13073-016-0294-z
4. Yoon MY, Yoon SS. Disruption of the Gut Ecosystem by Antibiotics. Yonsei Med J. 2018;59(1):4–12.doi:10.3349/ymj.2018.59.1.4
5. Bhalodi AA, van Engelen TSR, Virk HS, Wiersinga WJ. Impact of antimicrobial therapy on the gut microbiome. J Antimicrob Chemother. 2019; 74(Supplement_1):i6–i15. doi:10.1093/jac/dky530
Can Antibiotics Cause Other Health Problems?
Yes, they can and here is a short list:
In 1998 two scientists, Bernstein and Ross, discovered that antibiotics "significantly increased the risk of non-Hodgkin’s lymphoma in humans".
Asthma and Allergy Report (2001) states that the first immuno-deficiency syndrome was recognized in 1952. Since then, 95 more syndromes have been identified with newer conditions being discovered every day. The report also states that increased use of antibiotics in infancy contributes to elevated risks of allergies. It was in the 1950s that antibiotics came into widespread use in medicine. Do you see a correlation here?
In 2016, Aalto University in Finland published a study linking the childhood use of antibiotics to the development of asthma, inflammatory bowel diseases, diabetes, and obesity later in life.(Source)
In a study published in Genome Medicine (2016), Amy Langdon, Nathan Crook, and Gautam Dantas from the Washington University School of Medicine demonstrated that antibiotic use can also lead to Clostridium difficile infection, claiming the lives of about 14,000 people annually due to severe dysbiosis of human microbiome.
Dysbiosis is when the normal bacterial composition (85% good bacteria vs. 15% bad bacteria), gets thrown out of balance. In general, the numbers of dominating species decline while those of the restricted species rise.
Dysbiosis of the microbiome has been associated with a large number of health problems; with causal implications in metabolic, immunological, and developmental disorders. What’s more, dysbiosis is also linked to susceptibility towards development of infectious diseases.(Source)
A study published in the Nucleic Acid Research in 2018 found that Ciprofloxacin inhibited the normal maintenance and transcription of mitochondrial DNA, diminishing the total mitochondrial energy production.(Source)
And without energy, your cells can't function.
Dr. Vibhuti Rana, PhD says...
It is rightly stated that antibiotics are a root cause of several other health issues, including severe allergies. A few problems which accompany the antibiotic therapy include severe digestive issues, fungal issues in the vagina, throat, and mouth, skin problems like photosensitivity, etc. A study conducted in 1994 and published in CHEST demonstrated that the penicillin group antibiotics showed a higher frequency of allergic reactions and hypersensitivity than those belonging to cephalosporins in patients with cystic fibrosis (6).
Another study published in 2002 used Comet Assay to prove that
antibiotics induced DNA damage, hence impaired immune response in
malnourished children (7).
6. Roy A. Pleasants; Terrence R. Walker; Wayne M. Samuelson. Allergic reactions to parenteral beta-lactam antibiotics in patients with cystic fibrosis. Chest 1994, Vol: 106, Issue: 4, Page: 1124-8.
7. González, C., Nájera, O., Cortés, E., Toledo, G., López, L., Betancourt, M. and Ortiz, R. (2002), Susceptibility to DNA damage induced by antibiotics in lymphocytes from malnourished children. Teratog. Carcinog. Mutagen., 22: 147-158. doi:10.1002/tcm.10007.
Other Sources of Antibiotics
Antibiotics are also present in many common foods that most of us eat. More recently, Harvard Medical School found that antibiotics are now being detected in the water supply from our overuse. The waste water enters the sewer system, which is then treated, and in many cases pumped right back into the underground water table, rivers or lakes.(Source)
In the US, the most common foods that have antibiotics in them are commercial beef, dairy, and poultry. The livestock industry administers antibiotics to their animals in order to deplete the hazardous bacteria and make the food safe for consumption. Moreover, they are also used to fatten the animals. A fat cow will sell more than a thin cow, won't it? Hence, these antibiotics end up being present in milk, cheese, and the meat as well.
This overexposure to the antibiotics is resulting in antibiotic resistance among the pathogens residing in the host, not to mention the long-term health effects on our children. Ultimately, it destroys the beneficial bacteria in your intestines, allowing a yeast infection to develop.
How Can You Prevent These Yeast Infections?
Now it would be a rare individual that could go through life without ever being prescribed an antibiotic. We are in no way advocating to not ever take them because they do save lives. But choose wisely, do you really need to take them or not for whatever it is you have at the time?
Colds for instance are caused by a virus and the best way to treat them is to dry them out. We find that Mucinex during the day and Advil PM at bedtime does this quite well. By drying out the mucous you will be able to breath and will feel much better. Then it typically, for most people, takes two weeks to run its course.
Bladder and urinary tract infections are a very common reason women have to take antibiotics. On this webpage, we have a couple suggestions that I would try first before you committed to taking antibiotics. Rarely do our suggestions not work.
If you do decide to take an antibiotic, talk to your doctor about taking Nystatin and Fluconazole with it to avoid
the possible overgrowth of yeast. Just so you know, Nystatin works best in the intestine and Fluconazole, because it absorbs into the blood stream so well, works everywhere else.
You could get on a good high dose probiotic
product like those we talk about on this webpage. Whatever probiotic you choose, the probiotics help offset the antibiotic caused destruction of your good bacteria and
to help your good bacterial colonies replenish themselves. Doses should
be a minimum 50 billion twice a day and the stronger the antibiotic, the more you should take.
While on the antibiotic do not take the probiotic at the same time of day. Usually antibiotics are taken with food so take your probiotic 60 minutes before breakfast and at bedtime. When you are done with the antibiotic, take the probiotic away from meals on an empty stomach with non-chlorinated water for at least another three months so your microbiome you can fully recover.
To avoid antibiotics in meats, buy organic and grass fed beef. Not only is the fatty acid ratio correct, which will give you better health, but you will be avoiding the antibiotics as well.
What to Do if You Do Get a Yeast Infection?
When you take an antibiotic orally, you must be aware that it has stripped the good bacteria in your vagina and given you a yeast infection. Therefore, based on the points noted above, we know that it has reduced the friendly bacteria levels in your gut.
So the best thing to do is to fix the gut and the vaginal infections simultaneously, so that you can prevent recurrent infections and get back to normal in the shortest amount of time.
You can either see your doctor for an anti-fungal prescription, or do the basic yeast cleanse on this webpage while also treating the vaginal infection with these suggestions at the same time.
Dr. Vibhuti Rana, PhD says...
In today’s lifestyle, we are unknowingly consuming antibiotics via food and milk. Though we can’t help it, certain lifestyle and diet changes will help us in the long run to combat antibiotic-associated fungal infections. Use of probiotics is the most important compensatory measure for restoring the internal microflora damage. The suggestions given in this section are efficient in wiping unwanted yeast infection and give relief from frequent visits to the doctor. People with high sugar levels must keep their sugar intake under check, apart from maintaining healthy, clean, and dry skin (8).
In women with urogenital infections, probiotics are believed to be
the major treatment approach (9,
10). In summary, the use of “good bacteria” to boost
bacterial populations is steadily achieving scientific approval in
the form of probiotic therapy.
8. Candidiasis What Is It? Harvard Medical School. Published January, 2019
9. Reid G, Bruce AW. Urogenital infections in women: can probiotics help? Postgraduate Medical Journal 2003;79:428-432.
10. Reid G; Dols J, Miller W. Targeting the vaginal microbiota with probiotics as a means to counteract infections. Current Opinion in Clinical Nutrition and Metabolic Care 2009; 12 (6); 583-587. doi: 10.1097/MCO.0b013e328331b611
In Conclusion:
The bottom line is, antibiotic usage indirectly promotes yeast infections and if taken too often, yeast infections can become chronic and never go away, because they can severely alter your microbiome. In some cases it can take months of good diet, high dose probiotics, and anti-fungal agents to recover from the impact of antibiotics.
Medically Reviewed by Dr. Atmika Paudel, PhD
It is very well mentioned in the above article about how unnecessary and overuse of antibacterial agents can compromise our health by altering our gut microbiome. I would like to add here that the prolonged use of antibacterial agents not only alters the microbiome by killing good bacteria but also leads to a weakened immune system (1).
The overuse of antibacterial agents will harm macrophages, which fight against pathogenic microorganisms by engulfing them. The macrophages do not have the same ability to tackle with the infecting microorganisms when they are under the stress of antibacterial agents. Therefore there are two consequences: one is the opportunity for the yeasts to outgrow in the absence of bacteria in the gut, and the other is the opportunity for the yeasts to establish infection in the absence of the competent immune system of the host.
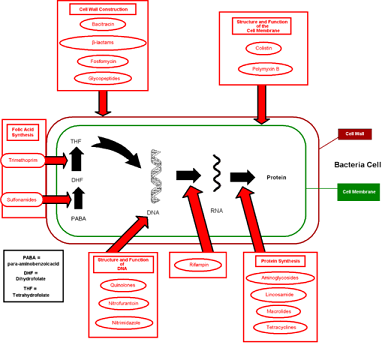
The bacterial cell and fungal/yeast cell are quite different; fungi are eukaryotes while bacteria are prokaryotic microorganisms. While most of the antibacterial agents target bacterial cell walls or specific structures conserved among bacteria, fungal cell wall structure is entirely different, so the antibacterial agents cannot interact with the cell wall, cannot pass through it, and fungi are not affected by the antibacterial agents. In fact, many of the antibacterial agents are produced by fungi and purified for use as medicine to treat bacterial infections.
It is obvious that in the absence of bacteria, there will be no competition for food and space inside the host for the fungi; they can grow and occupy space and consume the food without any struggle. The increased growth, together with the weak immune system, will then pave a platform for the yeasts to establish infection. Therefore, antibacterial agents should be saved for situations when they are absolutely necessary, not in the undesired cases such as a common cold.
(1) Yang JH, Bhargava P, McCloskey D, Mao N, Palsson BO, Collins JJ. Antibiotic-Induced Changes to the Host Metabolic Environment Inhibit Drug Efficacy and Alter Immune Function. Cell Host Microbe. 2017 Dec 13;22(6):757-765.e3. doi: 10.1016/j.chom.2017.10.020. Epub 2017 Nov 30.
Have Any Questions About Antibiotics?
Do you have any questions about antibiotics, how to repair the damage they cause, or yeast infections in general? Ask your question here or contact us using the contact page of this website. It is also always a good idea to talk to your doctor as well.
Back to Antibiotics Cause Yeast Home
Home Privacy Policy Copyright Policy Disclosure Policy Doctors Store
Copyright © 2003 - 2025. All Rights Reserved under USC Title 17. Do not copy
content from the pages of this website without our expressed written consent.
To do so is Plagiarism, Not Fair Use, is Illegal, and a violation of the
The Digital Millennium Copyright Act of 1998.